Neuropathy refers to the conditions that result when nerves that carry messages to and from the brain and spinal cord from and to the rest of the body are damaged or diseased. About 60-70% of people who have diabetes may have some form of diabetic neuropathy. This risk increases with age and the duration of diabetes. Generally people who have diabetes for at least 25 years are at the greatest risk.
 Diabetic neuropathy occurs when the tiny nerves in your body become damaged due to high blood sugars. It happens to around two-thirds of diabetics and can place you at risk for wounds and infections. The worst complication is amputation. If you have diabetic neuropathy, it is never too late to slow the effects and prevent complications!
Diabetic neuropathy occurs when the tiny nerves in your body become damaged due to high blood sugars. It happens to around two-thirds of diabetics and can place you at risk for wounds and infections. The worst complication is amputation. If you have diabetic neuropathy, it is never too late to slow the effects and prevent complications!
Diabetic Neuropathy: Types
There are a few different types of diabetic neuropathy. Depending on what type you have, your symptoms and the location of symptoms may differ. The different types of neuropathy include:
- Peripheral Neuropathy – This is the most seen neuropathy and affects your; hands, feet, arms, and legs.
- Autonomic Neuropathy – This type affects the nerves inside your body and includes the; stomach, lungs, eyes, sex drive, ability to sweat, bladder function, and bowels. It may also cause problems with your blood pressure and heart.
- Focal Neuropathy – While most neuropathy causes loss of feeling from the nerves, this type can cause weakness in the muscles near the affected nerve. It can also be quite painful.
- Proximal Neuropathy – Proximal neuropathy can cause weakness in the legs, with pain in your; buttocks, thighs, and hip areas.
Diabetic Neuropathy: Causes
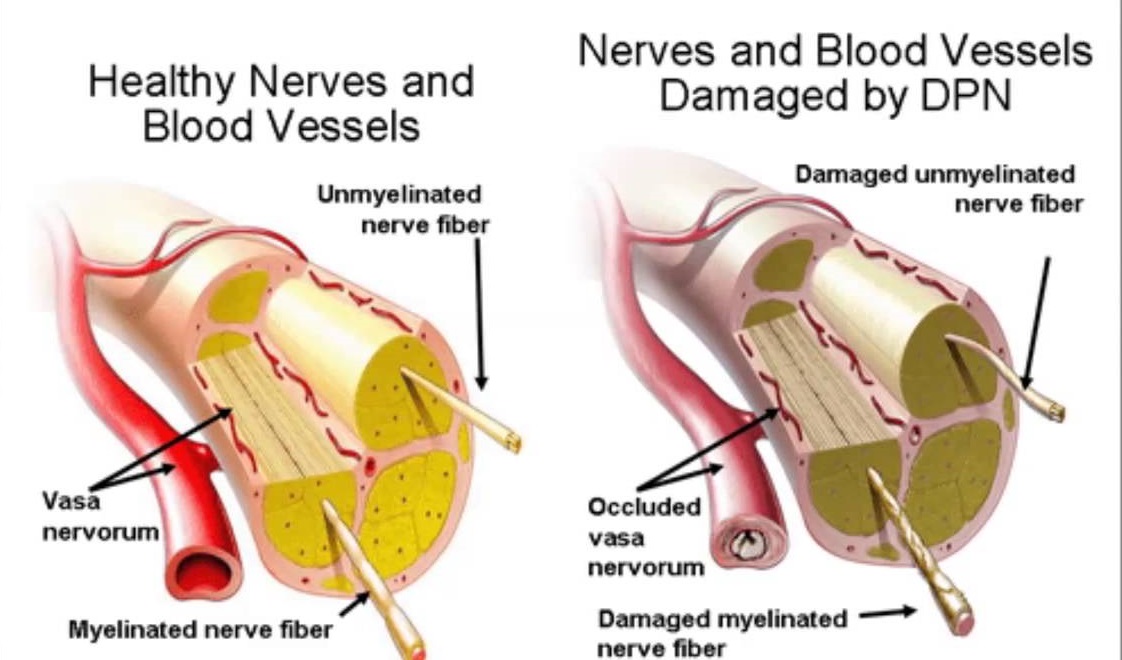
Diabetic neuropathy is caused by high blood sugars over a long period of time. The blood vessels and nerves are tiny and easily damaged. When the blood circulates, it brings them oxygen and nutrients to stay healthy. If there is too much blood sugar, this can damage them and cause them to die off. This results in loss of feeling to the feet, fingers, and extremities.
Other causes include:
- High Cholesterol
- Smoking
- Alcohol
- Autoimmune Disorders
- Family History of Neuropathy
- Injuries to Nerves
Diabetic Neuropathy: Symptoms
The different types of neuropathy each have their own set of symptoms. It just depends on what group of nerves have been affected by high blood sugars and possibly other factors. The important thing to understand is, diabetic neuropathy does not occur overnight and you may be suffering from it even without symptoms. As the damage gets worse, the symptoms will become more prominent.

Here are the symptoms according to the type of diabetic neuropathy:
Peripheral Neuropathy
If you have peripheral neuropathy, you will notice most of your symptoms in your extremities, most commonly your feet. Symptoms include:

- Numbness and Tingling
- Weakness in the Extremities
- Inability to Feel Pain or Temperature
- Cramps
- Muscle Twitches
- Achiness and Pain
- Sensitivity to Touch/Easily Tickled
Autonomic Neuropathy

If you have autonomic diabetic neuropathy, the nerves inside of your body are affected. This disrupts many of the functions that happen on their own like; eating and digesting your food, going to the bathroom, having sex, and blood pressure control. Symptoms of this type include:
- Feeling Dizzy
- Irregular Heartbeat
- Fainting
- Digestive Issues (Constipation, feeling bloated, Nausea, or Diarrhea)
- Blurred Vision, especially at night
- Sexual Problems
- Heavy Sweating or not enough
- Problems with Bowel or Bladder
- Hypoglycemia (Due to lack of symptoms when blood sugar drops)
Focal Neuropathy
This is a temporary type of neuropathy that happens suddenly then goes away. You may notice changes to your legs, mid-section, or your head. Watch for these symptoms:
- Chest Pain
- Abdominal Pain
- Lower Back Pain
- Side Pain
- Vision Issues
- Bell’s Palsy (Facial drooping on one side only)
- Leg, Thigh, or Foot Pain
Proximal Neuropathy
Proximal neuropathy may be lasting or temporary and affects your; legs, hips, thighs, and buttocks. The symptoms are:
- Problems Standing from Sitting
- Leg Weakness
Remember, diabetic neuropathy may come on very slowly and symptoms may not appear until the disease is in its more advanced stages. It is important to take note of any symptoms you may be feeling and let your doctor know if you have any changes.
Diabetic Neuropathy: How Can I Lead an Active Lifestyle?
You need to make sure that you check your feet and extremities for wounds or infection that may have occurred without you knowing. If you feel numbness or tingling in your extremities, let your doctor know right away. They can order tests on your nerves to see if they are working or damaged.
If you are diagnosed with diabetic neuropathy, these tips can help keep you active and help prevent complications:
- Take Good Care of your Feet and Legs

Foot damage due to diabetes can result in foot ulcers, infection, etc. This is mainly due to 2 reasons-
First is due to loss of sensation from nerve damage. You may not pay attention to a small sore or ulcer as you can’t feel the pain. These ulcers, if untreated, can get infected, sometimes leading to serious infection (cellulitis) and in extreme situations, may require you to have that part of the foot or leg amputated.
The second issue is poor circulation. Uncontrolled diabetes for years will lead to narrowing of your blood vessels which can increase the risk of foot ulcers. The risk is particularly worse if you are a smoker.
For example, more than 60% of non-traumatic (not caused by accidents) leg amputations in the US are due to diabetes. Research has shown that if you take care of your feet well, it can reduce amputation rates by 45 to 85 percent.
Here are some ways you can take of your feet when you have diabetes-
- Keep the feet clean- Clean the feet daily using warm—not hot—water and a mild soap. Soaking the feet should be avoided. A soft towel can be used to dry the feet and between the toes.
- Inspecting the feet and toes every day for cuts, blisters, redness, swelling, calluses, or other problems. Using a mirror—handheld or placed on the floor—may be helpful in checking the bottoms of the feet, or another person can help check the feet. A health care provider should be notified of any problems.
- Lotion to moisturize the feet. Getting lotion between the toes should be avoided.
- Filing corns and calluses gently with a pumice stone after a bath or shower.
- Cutting toenails to the shape of the toes and filing the edges with an emery board each week or when needed.
- Wearing shoes or slippers all the time to protect feet from injuries. Wearing thick, soft, seamless socks can prevent skin irritation.
- Wearing shoes that fit well and allow the toes to move. New shoes can be broken in gradually by first wearing them for only an hour at a time.
- Looking shoes over carefully before putting them on and feeling the insides to make sure the shoes are free of tears, sharp edges, or objects that might injure the feet.
People who need help taking care of their feet should consider making an appointment to see a foot doctor, also called a podiatrist.
- Keep Blood Sugar Under Control
Work hard to keep your blood sugar under strict control. Ask your doctor for acceptable ranges and work hard to keep within those guidelines. This will also help protect the tiny blood vessels in your eyes and other areas of your body.
- Eat Healthy
You can help maintain a healthy blood sugar level by eating right. Make sure you avoid junk or fast food, and eat healthy fresh foods prepared at home. Try to cut out excess carbohydrates and beverages with high fructose corn syrup. ncluding plenty of fiber in your diet will also help and make sure you include healthy fats like Omega-3 Fatty Acids, Avocado, and Nuts. These also help improve circulation and blood flow to the extremities.
- Get Moving
Activity can help reduce your blood sugar levels and get the blood flowing in your body. This is one way you can continue to have an active lifestyle with diabetic neuropathy and keep it under control. Make sure if you exercise that you have proper footwear, and permission from your doctor before you start. Good ideas for activity include:
- Walking
- Swimming
- Yoga
- Riding a Bike
- Gentle Stretches
- Weight Training
If you decide to exercise or increase your activity, it is important to check your blood sugar before, during, and after exercise. It is possible to experience hypoglycemia as your body gets used to more activity. Always have sugar rescue or a snack handy.
- Make Healthy Lifestyle Changes
Certain lifestyle factors increase your risk of diabetic neuropathy. If you drink alcohol, try to drink in moderation keeping it to one to two drinks per day. If you smoke, now is the time to try and quit. Also, make sure you decrease your exposure to toxic fumes, household cleaners, and pesticides. There are plenty of all-natural solutions for these products that have less impact on the environment and your body.
How is Diabetic Neuropathy Diagnosed?
Doctors diagnose neuropathy based on your symptoms and a physical exam.
During the exam, the doctor may also check blood pressure, heart rate, muscle strength, reflexes, and sensitivity to position changes, vibration, temperature, or light touch.
Foot Exams
If you have diabetes, have your feet checked for peripheral neuropathy by a health care provider every year.
People diagnosed with peripheral neuropathy need more frequent foot exams.
A comprehensive foot exam assesses the skin, muscles, bones, circulation, and sensation of the feet.
Your doctors may perform foot exam every year to check your sensation or feeling in the feet with a nylon brush or by pricking them with a pin. They may also check your ability to sense the temperature or may use a tuning fork to check your ability to feel the vibration.
Other Tests
The doctor may perform other tests as part of the diagnosis.
- Nerve conduction studies and electromyography are sometimes used to help determine the type and extent of nerve damage. Nerve conduction studies check the transmission of electrical current through a nerve. Electromyography shows how well muscles respond to electrical signals transmitted by nearby nerves. These tests are rarely needed to diagnose neuropathy.
- A check of heart rate variabilityshows how the heart responds to deep breathing and to changes in blood pressure and posture.
- Ultrasounduses sound waves to produce an image of internal organs. An ultrasound of the bladder and other parts of the urinary tract, for example, can be used to assess the structure of these organs and show whether the bladder empties completely after urination
Diabetic Neuropathy: Treatment
As mentioned before, strict blood sugar control is very important to prevent any more nerve damage. Sometimes you may need medications depending on your symptoms and what nerves are damaged.
Pain Relief
There are several medications available to treat diabetic nerve pain if that is your main symptoms. Sometimes you may need a combination of medications or treatments and should consider talking with your health care provider about treatment options.
Oral medications used to help relieve diabetic nerve pain include-
- Anti depressants: People do not have to be depressed for an antidepressant to help relieve their nerve pain. There are several options here including Tricyclic antidepressants, such as amitriptyline (Elavil), imipramine, and desipramine (Norpramin, Pertofrane). Other types of antidepressants, such as duloxetine (Cymbalta), venlafaxine, bupropion (Wellbutrin), paroxetine (Paxil), and citalopram (Celexa)
- Anticonvulsants: Pregabalin (Lyrica), gabapentin (Gabarone, Neurontin), carbamazepine, and lamotrigine (Lamictal)
- Pain killers: Pain medications such as Tramnadol, Oxycodone, etc.
Duloxetine (Cymbalta) and pregabalin (Lyrica) are approved by the U.S. Food and Drug Administration specifically for treating painful diabetic peripheral neuropathy.
All medications have side effects, and some are not recommended for use in older adults or those with heart disease. Because over-the-counter pain medicines such as acetaminophen and ibuprofen may not work well for treating most nerve pain and can have serious side effects, some experts recommend avoiding these medications.
Topical treatments that are applied to the skin—typically to the feet—include capsaicin cream and lidocaine patches (Lidoderm, Lidopain). Studies suggest that nitrate sprays or patches for the feet may relieve pain. Studies of alpha-lipoic acid, an antioxidant, and evening primrose oil suggest they may help relieve symptoms and improve nerve function in some patients.
A device called a bed cradle can keep sheets and blankets from touching sensitive feet and legs.
Alternative treatments: Acupuncture, biofeedback, or physical therapy may help relieve pain in some people. Treatments that involve electrical nerve stimulation, magnetic therapy, and laser or light therapy may be helpful but need further study.
Gastrointestinal Problems
To relieve mild symptoms of gastroparesis—indigestion, belching, nausea, or vomiting—doctors suggest eating small, frequent meals; avoiding fats; and eating less fiber. When symptoms are severe, doctors may prescribe erythromycin or metoclopramide (Reglan) to speed digestion and help relieve nausea, or other medications to help regulate digestion or reduce stomach acid secretion.
To relieve diarrhea or other bowel problems, doctors may prescribe an antibiotic such as tetracycline, or other medications as appropriate.
Dizziness and Weakness
Sitting or standing slowly may help prevent the light-headedness, dizziness, or fainting associated with blood pressure and circulation problems. Raising the head of the bed or wearing elastic stockings may also help. Some people benefit from increased salt in the diet and treatment with salt-retaining hormones. Others benefit from high blood pressure medications. Physical therapy can help when muscle weakness or loss of coordination is a problem.
Urinary and Sexual Problems
To clear up a urinary tract infection, the doctor will probably prescribe an antibiotic. Drinking plenty of fluids will help prevent another infection. People who have incontinence should try to urinate at regular intervals—every 3 hours, for example—because they may not be able to tell when the bladder is full.
To treat erectile dysfunction in men, the doctor will first do tests to rule out a hormonal cause. Several methods are available to treat erectile dysfunction caused by neuropathy. Medicines are available to help men have and maintain erections by increasing blood flow to the penis. Some are oral medications and others are injected into the penis or inserted into the urethra at the tip of the penis. Mechanical vacuum devices can also increase blood flow to the penis. Another option is to surgically implant an inflatable or semirigid device in the penis.
Vaginal lubricants may be useful for women when neuropathy causes vaginal dryness. To treat problems with arousal and orgasm, the doctor may refer women to a gynecologist.
You may think that diabetic neuropathy will limit your lifestyle as a diabetic. However, it is possible to live an active and full life if you take care of yourself.
__________________________________________________________________________________
Source:
- https://www.niddk.nih.gov/health-information/diabetes/preventing-diabetes-problems/nerve-damage-diabetic-neuropathies.
