Diabetes can cause eye problems, over time this can even lead to blindness unless take precautions. Unfortunately, many people with diabetes do not have eye exams or not aware that they need yearly eye exams. Although people with diabetes are at higher risk for eye complications, these can be prevented with tight blood sugar control.

Cataract
Cataract is a condition where there is clouding of the lens in the eye that affects the vision. People with diabetes are 60% more likely to develop cataract and also tend to get cataract at a younger age then people without diabetes. Cataract can be treated with eyeglasses if it is mild. Once it is advanced, this can be treated with surgically replacing the lens with artificial lens.
Glaucoma
Glaucoma is a condition where the pressure in the eye is increased. Due to the pressure, the fluid in the eye cannot be drained adequately. This results in excessive pressure on the optic nerve and the blood vessels that supply the regular. Over the years this can result in damage to the optic nerve and the retina resulting in decreased vision or blindness. The risk of glaucoma increases with age and also the length of time someone has diabetes. A person with the diabetes is nearly twice as likely to get glaucoma as other adults. If detected early, glaucoma can be treated effectively with either medications or surgery to prevent blindness.
Diabetic Retinopathy
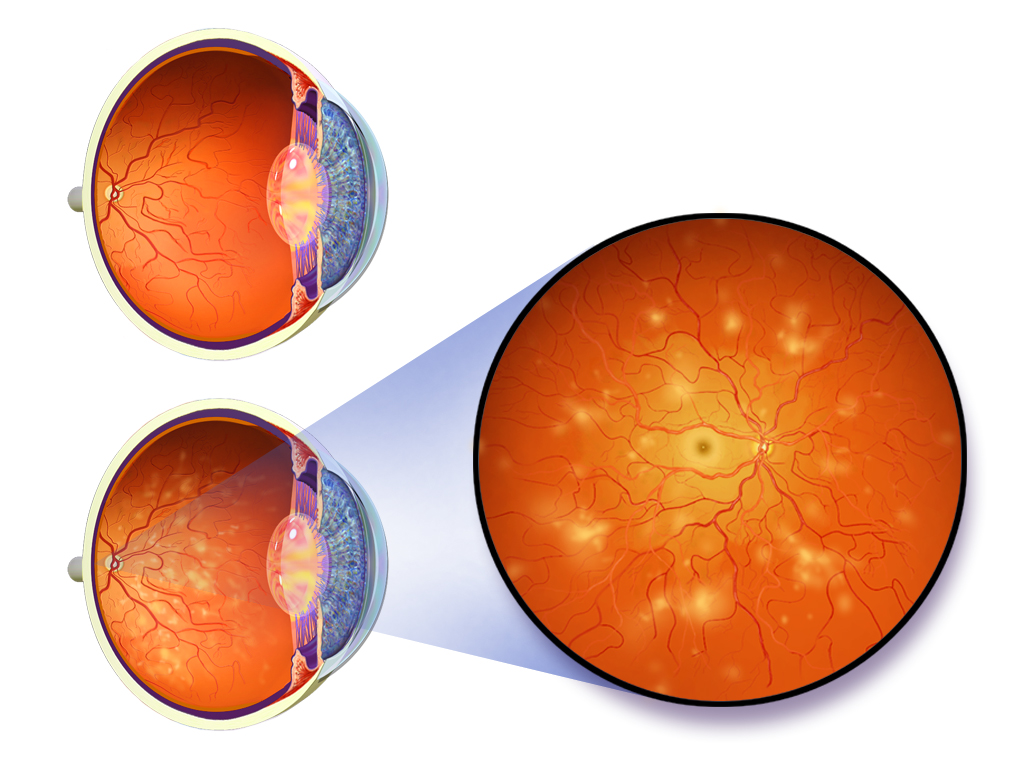
Retina is the light-sensitive tissue at the back of the eye. Retinopathy refers to eye disease that is caused by changes in blood vessels of the retina due to diabetes. Diabetic retinopathy is the most common diabetic eye disease and a leading cause of blindness in people with diabetes. During the initial stages of retinopathy, you may not have any vision changes but over a period it can slowly lead to vision loss. It usually affects both eyes. In some people with retinopathy, blood was also may swell and delete fluid. In other people, abnormal new blood vessels cut on the surface of the retina.
What are the symptoms of retinopathy?
In early stages, you may not have any symptoms. As the disease progresses, he may see “floaters” or may see few red spots.
Different stages of diabetic retinopathy:
- Mild nonproliferative retinopathy. Small areas of balloon-like swelling in the retina’s blood vessels.
- Moderate nonproliferative retinopathy. Some blood vessels that supply the retina are blocked.
- Severe nonproliferative retinopathy. More blood vessels are blocked. This will result in the body to grow new blood vessels for nourishment.
- proliferative retinopathy. This is an advanced age with the signal sent by the retina for nourishment triggered the growth of new blood vessels. These blood vessels are abnormal and fragile. If these blood vessels leak blood, severe vision loss and even blindness can occur.
Who is at risk and what can you do to prevent diabetic retinopathy?
All people with diabetes are at risk for diabetic retinopathy. Almost half of people who have diabetes have some stage of diabetic retinopathy. It is recommended that a diabetic should have a comprehensive dilated eye exam at least once a year. If they already have diabetic retinopathy, they may need eye exam more often. Better control of blood sugar can slow the onset and progression of retinopathy.
What other treatment options for diabetic retinopathy?
No treatment is needed for early stages of diabetic retinopathy other than controlling blood sugar, cholesterol and blood pressure.
When you have advanced retinopathy, laser treatment can be done to shrink the abnormal new blood vessels. However, if these blood vessels started bleeding, you may need a surgical procedure called vitrectomy where blood is removed from the center of your eye.
There are some medications that are being used to treat diabetic retinopathy. These medications are injected into the eye to slow down the growth of new blood vessels in the retina. But these medications are considered investigational and generally used along with the laser treatment or with vitrectomy.

2 thoughts on “Diabetic Eye Disease”