Diabetes, especially if it is uncontrolled can cause multiple complications. The digestive system is no exception. Some of the diabetes complications can happen if you have diabetes for a long time or it depends on what type of diabetes you have. Digestive complications can happen if diabetes is not controlled even for a short period of time. So, it is important to know that most of these complications are preventable and sometimes reversible when you control your blood sugars well.
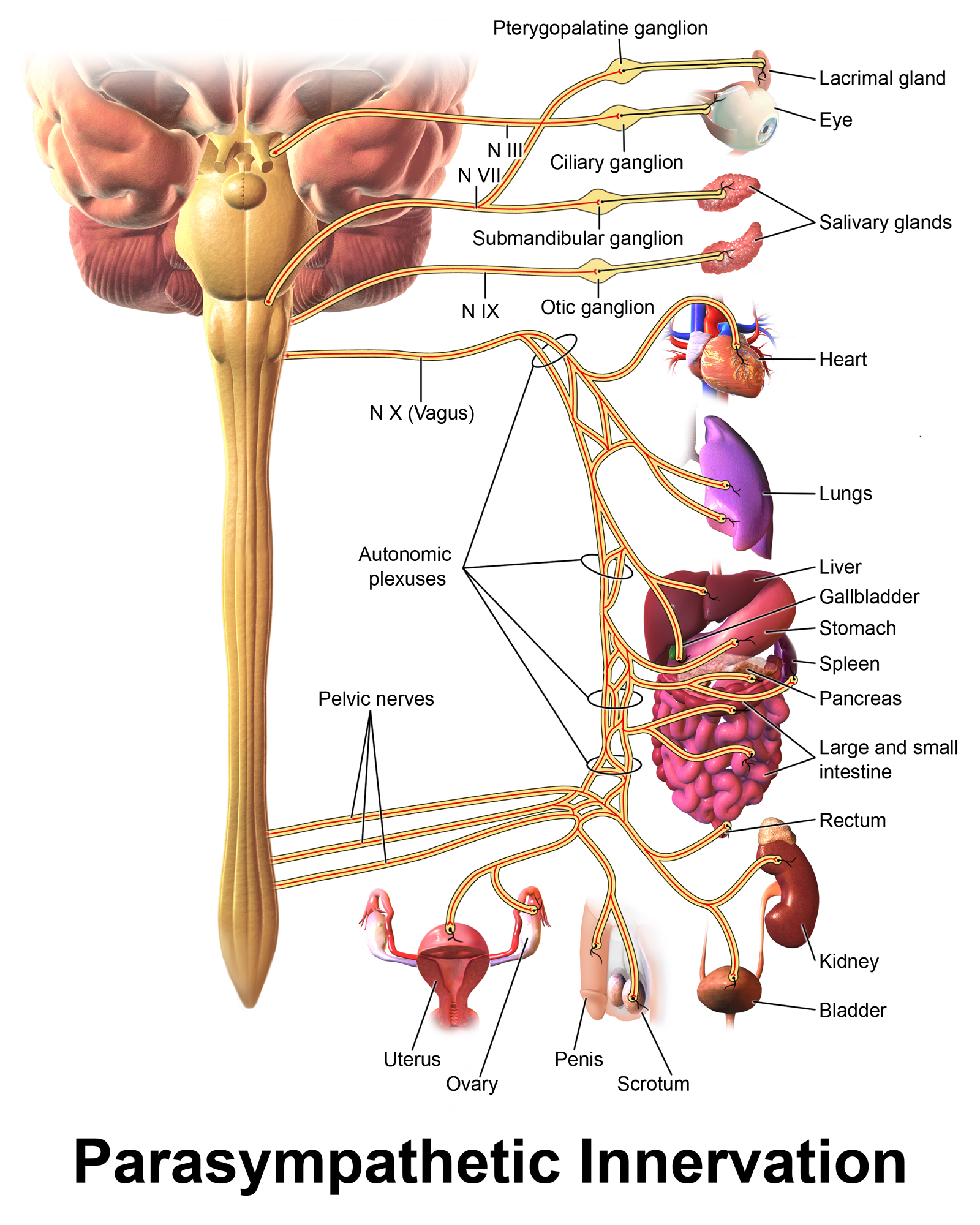
Autonomic neuropathy is the main culprit
Autonomic neuropathy is damage to the nerves that regulate the body functions that a person doesn’t have control including the nerves that control your heart rate, digestion, blood pressure, sweating, etc. This nerve damage interferes with the messages sent between the brain and other organs. Diabetes is one of the most common causes of this kind of nerve damage.
Diabetes affects digestive system in many ways-
- Gastroparesis
- GERD
- Fatty liver
- Diarrhea
- Constipation
- Celiac disease
- Pancreatitis or pancreatic cancer
Gastroparesis
The nerve damage around the stomach can make the stomach (gastro) to slow down (paresis) . This affects the processing of the food and causes delay of the food passing through the stomach into the small intestine. Gastroparesis causes the food to stay in the stomach longer than usual resulting in nausea, vomiting, bloating, abdominal pain and feeling too full even with small meals.
Gastroparesis is the most common digestive system complication of diabetes. It affects approximately 1% of the people with type 2 diabetes and up to 5% of people with type 1 diabetes. People who have type 2 diabetes and are obese are at even higher risk of developing gastroparesis. Gastroparesis can be very debilitating especially when it is severe.
Your healthcare provider can make a diagnosis of gastroparesis by doing a test called gastric emptying scan. This nuclear medicine scan will be able to confirm if you have gastroparesis.
Prevention is better than cure.
- Diabetic gastroparesis generally occurs when you have prolonged periods of uncontrolled blood sugars. So, the key is to have strict blood sugar controls.
- Smaller, more frequent meals, up to 6-8 per day. You will be able to tolerate semisolid or liquid form of foods better than solid foods.
- Avoid fatty foods and high-fiber foods.
- Avoid medications that may delay gastric emptying including pain medication, some acid reducers, blood pressure medications, Benadryl, etc.
There are only a few medications that are effective in treating gastroparesis.
If you’re still having symptoms of gastroparesis in spite of following the diet strictly and if your blood sugars are controlled well, then you may need medications.
Metoclopramide (Reglan) is the only medication that is approved by FDA to treat gastroparesis. Because of the side effects, this medication is generally not used long-term. Domperidone and erythromycin are the other 2 drugs sometimes used. Domperidone is considered an experimental drug requiring approval from FDA before that can be used in US.
If all else fails, there is a surgical procedure where they insert an electrical stimulator (like a pacemaker for the heart).
GERD
There is a valve between the lower part of the esophagus and stomach that prevents acid backing up into the esophagus. When there is autonomic nerve damage, this valve is not as tight allowing acid to back up into the esophagus causing heartburn, regurgitation of food, chronic cough, difficulty swallowing, etc.
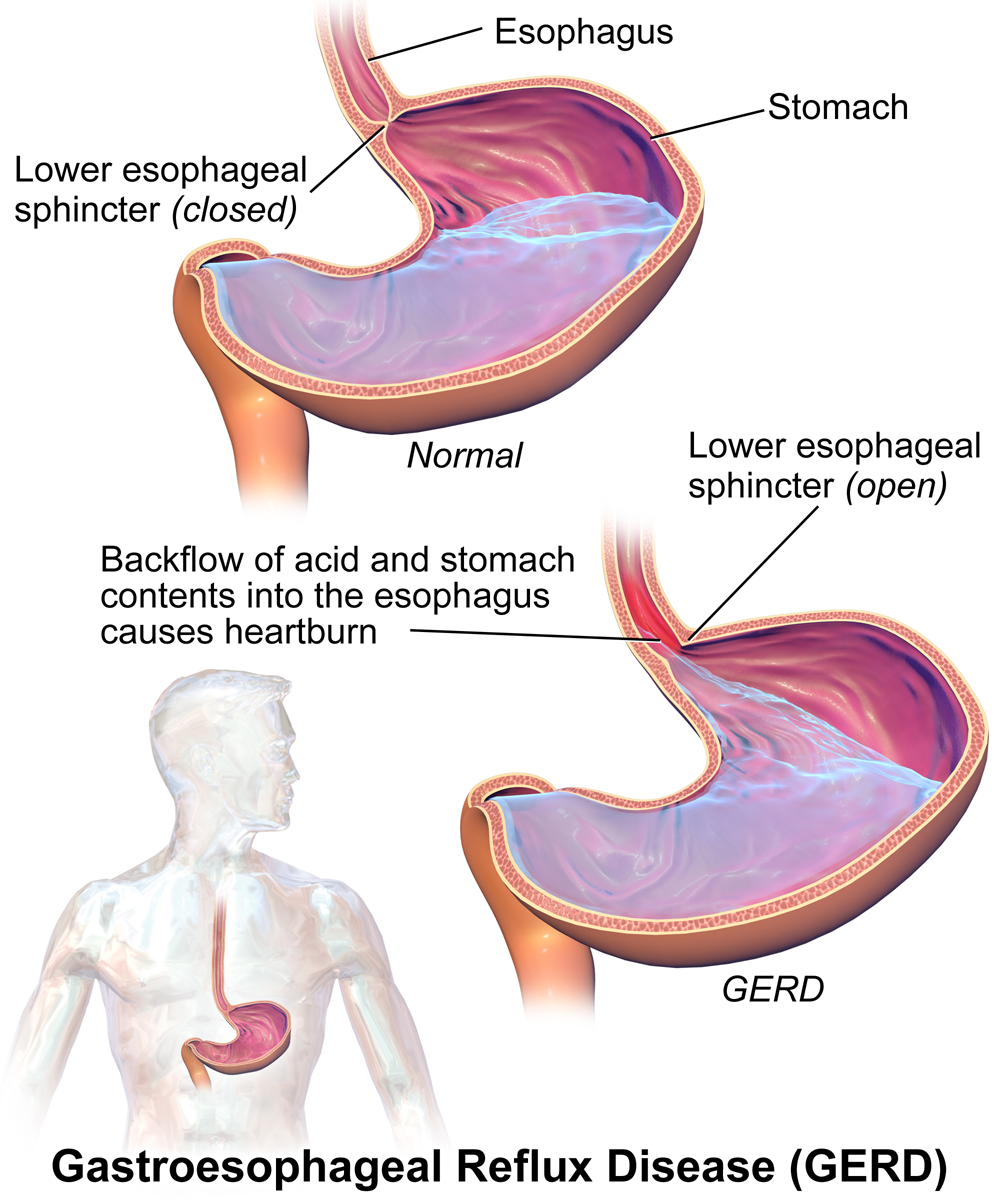
The treatment of GERD mainly involves diet and lifestyle changes.
If you’re overweight, the first step would be to try to lose weight which helps acid reflux tremendously.
There are several foods that can trigger acid reflux symptoms including fatty or greasy foods, caffeine, alcohol, chocolate, tomato sauce, etc. these foods should be minimized or avoided.
Smoking cessation also helps.
If you have acid reflux at least 3-4 times a week, then you need to talk to your health care provider to see if you need medications. Sometimes he may need endoscopy evaluation to see if there is any damage to the esophagus especially if you’re also experiencing difficulty swallowing.
Liver disease
Fatty liver, or steatosis, is a term that describes the buildup of fat in the liver. Although it is normal to have some amount of fat in your liver, if it makes up more than 5%-10% of your liver weight, you may have fatty liver.
Fatty liver is caused by number of risk factors including alcohol, obesity, diabetes, genetic factors, etc.,
In a small percentage of people, fatty liver can cause severe scarring of the liver and cirrhosis. Approximately 30% of the US population has fatty liver. If you have diabetes or if you’re overweight, the risk may be much higher.
About two thirds of patients above 50 years of age who have diabetes and obesity may have severe fatty liver disease associated with inflammation and scarring called non-alcoholic steatohepatitis (NASH)
Insulin resistance is a major factor causing excessive fat accumulation in the liver. Since diabetes is also due to insulin resistance, it is thought that fatty liver may be a complication of type 2 diabetes or vice versa.
Ultrasound of the liver can confirm if you have fatty liver not. Just having fatty liver does not always mean that it will lead to liver damage unless there is inflammation in the liver. This can be checked by having liver enzyme tests done. If you do have abnormal liver enzymes, then you need to focus on reversing the fatty liver.
Weight loss and strict blood sugar control are very important when you have fatty liver. There are some medications such as Metformin, Pioglitazone (Actos), Atorvastatin (Lipitor), vitamin E, etc. that may be effective in decreasing the inflammation and sometimes even reversing the fatty liver.
Diabetic diarrhea
Diabetic diarrhea can be due to multiple reasons- autonomic nerve damage causing problem with the motility of small intestine or it could be due to too much fluid secreted by the lining of your bowels.
Diabetic diarrhea may also be caused by some of the medications you take for diabetes such as metformin or it could be due to artificial sweeteners such as sorbitol.
Whenever you have diarrhea that lasts more than a few weeks, you need to be evaluated by your physician to make sure that the cause of the diarrhea is determined.
Generally the treatment of diarrhea really depends on what is causing it in the first place.
Due to altered motility, sometimes people can have overgrowth of small intestinal bacteria that may require antibiotics.
People with type 1 diabetes are more prone to have celiac disease that needs to be ruled out. Sometimes pancreas damage can also cause diarrhea which your healthcare provider may be able to determine. To manage the diarrhea, sometimes you may need to use over-the-counter or prescription anti-diarrheal medicines.
Celiac disease
Patients with type 1 diabetes have at least 5-10 times higher risk of having celiac disease. So, if you have type 1 diabetes and start having any digestive symptoms such as abdominal pain, diarrhea, weight loss, etc., you may need to discuss with your health care provider to check for celiac disease by doing a blood test.
Pancreatitis and pancreatic cancer
Diabetes can sometimes puts you at higher risk for inflammation of the pancreas called pancreatitis. Diabetes is also linked with an increased risk of pancreatic cancer, particularly if you’re recently diagnosed with diabetes.
