Fall in your sugar levels or hypoglycemia is more of an abrupt phenomenon rather than gradual and it should be taken very seriously. If your sugar level falls below 70mg/dL, you are in hypoglycemia. It is usually mild and can be treated quickly and easily by eating or drinking a small amount of glucose-rich food. If left untreated, hypoglycemia can get worse and causes confusion, clumsiness, or fainting. Severe hypoglycemia can lead to seizures, coma, and even death.
Signs and Symptoms of Hypoglycemia
The onset of hypoglycemia can be very sudden and it can be a very frightening and dangerous condition. That’s because all our body cells work by getting energy from glucose present in the blood including our brain cells.
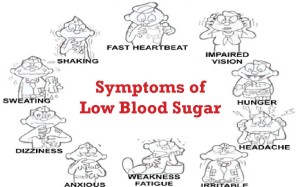 Hypoglycemia causes symptoms such as-
Hypoglycemia causes symptoms such as-
- hunger
- shakiness
- nervousness
- sweating
- dizziness or light-headedness
- sleepiness
- confusion
- difficulty speaking
- anxiety
- weakness
- blurred vision
Hypoglycemia can also happen during sleep and can have following signs-
- crying out or having nightmares
- finding pajamas or sheets damp from perspiration
- feeling tired, irritable, or confused after waking up
Factors causing hypoglycemia
Diabetes Medications
Hypoglycemia can occur as a side effect of some diabetes medications, including insulin and oral diabetes medications—pills—that increase insulin production, such as
- chlorpropamide (Diabinese)
- glimepiride (Amaryl)
- glipizide (Glucotrol, Glucotrol XL)
- glyburide (DiaBeta, Glynase, Micronase)
- nateglinide (Starlix)
- repaglinide (Prandin)
- sitagliptin (Januvia)
- tolazamide
- tolbutamide
Certain combination pills can also cause low blood sugars, including
- glipizide + metformin (Metaglip)
- glyburide + metformin (Glucovance)
- pioglitazone + glimepiride (Duetact)
- rosiglitazone + glimepiride (Avandaryl)
- sitagliptin + metformin (Janumet)
Other types of diabetes pills, when taken alone, do not cause hypoglycemia. Examples of these medications are
- acarbose (Precose)
- metformin (Glucophage)
- miglitol (Glyset)
- pioglitazone (Actos)
- rosiglitazone (Avandia)
However, taking these pills along with other diabetes medications—insulin, pills that increase insulin production, or both—increases the risk of hypoglycemia.
In addition, use of the following injectable medications can cause hypoglycemia:
- Pramlintide (Symlin), which is used along with insulin
- Exenatide (Byetta), which can cause hypoglycemia when used in combination with chlorpropamide, glimepiride, glipizide, glyburide, tolazamide, and tolbutamide
Other factors Causing hypoglycemia
- Excessive stress and exertion can cause your sugar levels to fall gradually or suddenly depending on the amount of stress and your tolerance.
- Quick consumption of blood glucose from your body due to activities like excessive exercise than you usual routine, skipping meals, eating less and long time gaps between meals.
- Slow release of glucose into the bloodstream.
- Babies born to diabetic mothers are vulnerable to hypoglycemic conditions.
- Factors like consumption of alcohol and weight-loss surgeries can also cause drops in sugar levels.
- Diseases like heart, kidney and liver failure and severe infections can lead to low blood sugars.
- Tumors of pancreas like Insulinoma increases the amount of insulin present in the body, which reduces the availability of glucose in your blood.
- Hormonal abnormalities of Cortisol, glucagon and thyroid hormones can also result in the same.
- Diabetics always have a chance of developing severe hypoglycemic conditions in case of over-medication, or medicine taken empty stomach. Hence, they are advised to always carry glucose supplements like candies with them.
Managing the drops in sugar levels
Prompt Treatment for Hypoglycemia
When people think their blood glucose is too low, they should check the blood glucose level of a blood sample using a meter. If the level is below 70 mg/dL, one of these quick-fix foods should be consumed right away to raise blood glucose:
- 3 or 4 glucose tablets
- 1 serving of glucose gel—the amount equal to 15 grams of carbohydrate
- 1/2 cup, or 4 ounces, of any fruit juice
- 1/2 cup, or 4 ounces, of a regular—not diet—soft drink
- 1 cup, or 8 ounces, of milk
- 5 or 6 pieces of hard candy
- 1 tablespoon of sugar or honey
Recommended amounts may be less for small children. The child’s doctor can advise about the right amount to give a child.
The next step is to recheck blood glucose in 15 minutes to make sure it is 70 mg/dL or above. If it’s still too low, another serving of a quick-fix food should be eaten. These steps should be repeated until the blood glucose level is 70 mg/dL or above. If the next meal is an hour or more away, a snack should be eaten once the quick-fix foods have raised the blood glucose level to 70 mg/dL or above.
For People Who Take Acarbose (Precose) or Miglitol (Glyset)
People who take either of these diabetes medications should know that only pure glucose, also called dextrose—available in tablet or gel form—will raise their blood glucose level during a low blood glucose episode. Other quick-fix foods and drinks won’t raise the level quickly enough because acarbose and miglitol slow the digestion of other forms of carbohydrate.
Help from Others for Severe Hypoglycemia
Severe hypoglycemia—very low blood glucose—can cause a person to pass out and can even be life threatening. Severe hypoglycemia is more likely to occur in people with type 1 diabetes. People should ask a health care provider what to do about severe hypoglycemia. Another person can help someone who has passed out by giving an injection of glucagon. Glucagon will rapidly bring the blood glucose level back to normal and help the person regain consciousness. A health care provider can prescribe a glucagon emergency kit. Family, friends, or coworkers—the people who will be around the person at risk of hypoglycemia—can learn how to give a glucagon injection and when to call 911 or get medical help.
Physical Activity and Blood Glucose Levels
Physical activity has many benefits for people with diabetes, including lowering blood glucose levels. However, physical activity can make levels too low and can cause hypoglycemia up to 24 hours afterward. A health care provider can advise about checking the blood glucose level before exercise. For those who take insulin or one of the oral medications that increase insulin production, the health care provider may suggest having a snack if the glucose level is below 100 mg/dL or adjusting medication doses before physical activity to help avoid hypoglycemia. A snack can prevent hypoglycemia. The health care provider may suggest extra blood glucose checks, especially after strenuous exercise.
Hypoglycemia When Driving
Hypoglycemia is particularly dangerous if it happens to someone who is driving. People with hypoglycemia may have trouble concentrating or seeing clearly behind the wheel and may not be able to react quickly to road hazards or to the actions of other drivers. To prevent problems, people at risk for hypoglycemia should check their blood glucose level before driving. During longer trips, they should check their blood glucose level frequently and eat snacks as needed to keep the level at 70 mg/dL or above. If necessary, they should stop for treatment and then make sure their blood glucose level is 70 mg/dL or above before starting to drive again.
Hypoglycemia Unawareness
Some people with diabetes do not have early warning signs of low blood glucose, a condition called hypoglycemia unawareness. This condition occurs most often in people with type 1 diabetes, but it can also occur in people with type 2 diabetes. People with hypoglycemia unawareness may need to check their blood glucose level more often so they know when hypoglycemia is about to occur. They also may need a change in their medications, meal plan, or physical activity routine.
Hypoglycemia unawareness develops when frequent episodes of hypoglycemia lead to changes in how the body reacts to low blood glucose levels. The body stops releasing the hormone epinephrine and other stress hormones when blood glucose drops too low. The loss of the body’s ability to release stress hormones after repeated episodes of hypoglycemia is calledhypoglycemia-associated autonomic failure, or HAAF.
Epinephrine causes early warning symptoms of hypoglycemia such as shakiness, sweating, anxiety, and hunger. Without the release of epinephrine and the symptoms it causes, a person may not realize that hypoglycemia is occurring and may not take action to treat it. A vicious cycle can occur in which frequent hypoglycemia leads to hypoglycemia unawareness and HAAF, which in turn leads to even more severe and dangerous hypoglycemia. Studies have shown that preventing hypoglycemia for a period as short as several weeks can sometimes break this cycle and restore awareness of symptoms. Health care providers may therefore advise people who have had severe hypoglycemia to aim for higher-than-usual blood glucose targets for short-term periods.
How can hypoglycemia be prevented?
Diabetes treatment plans are designed to match the dose and timing of medication to a person’s usual schedule of meals and activities. Mismatches could result in hypoglycemia. For example, taking a dose of insulin—or other medication that increases insulin levels—but then skipping a meal could result in hypoglycemia.
To help prevent hypoglycemia, people with diabetes should always consider the following:
- Their diabetes medications. A health care provider can explain which diabetes medications can cause hypoglycemia and explain how and when to take medications. For good diabetes management, people with diabetes should take diabetes medications in the recommended doses at the recommended times. In some cases, health care providers may suggest that patients learn how to adjust medications to match changes in their schedule or routine.
- Their meal plan. A registered dietitian can help design a meal plan that fits one’s personal preferences and lifestyle. Following one’s meal plan is important for managing diabetes. People with diabetes should eat regular meals, have enough food at each meal, and try not to skip meals or snacks. Snacks are particularly important for some people before going to sleep or exercising. Some snacks may be more effective than others in preventing hypoglycemia overnight. The dietitian can make recommendations for snacks.
- Their daily activity. To help prevent hypoglycemia caused by physical activity, health care providers may advise
- checking blood glucose before sports, exercise, or other physical activity and having a snack if the level is below 100 milligrams per deciliter (mg/dL)
- adjusting medication before physical activity
- checking blood glucose at regular intervals during extended periods of physical activity and having snacks as needed
- checking blood glucose periodically after physical activity
- Their use of alcoholic beverages. Drinking alcoholic beverages, especially on an empty stomach, can cause hypoglycemia, even a day or two later. Heavy drinking can be particularly dangerous for people taking insulin or medications that increase insulin production. Alcoholic beverages should always be consumed with a snack or meal at the same time. A health care provider can suggest how to safely include alcohol in a meal plan.
- Their diabetes management plan. Intensive diabetes management—keeping blood glucose as close to the normal range as possible to prevent long-term complications—can increase the risk of hypoglycemia. Those whose goal is tight control should talk with a health care provider about ways to prevent hypoglycemia and how best to treat it if it occurs.
Being Prepared for Hypoglycemia
People who use insulin or take an oral diabetes medication that can cause low blood glucose should always be prepared to prevent and treat low blood glucose by
- learning what can trigger low blood glucose levels
- having their blood glucose meter available to test glucose levels; frequent testing may be critical for those with hypoglycemia unawareness, particularly before driving a car or engaging in any hazardous activity
- always having several servings of quick-fix foods or drinks handy
- wearing a medical identification bracelet or necklace
- planning what to do if they develop severe hypoglycemia
- telling their family, friends, and coworkers about the symptoms of hypoglycemia and how they can help if needed.
Source: https://www.niddk.nih.gov/health-information/health-topics/Diabetes/hypoglycemia
